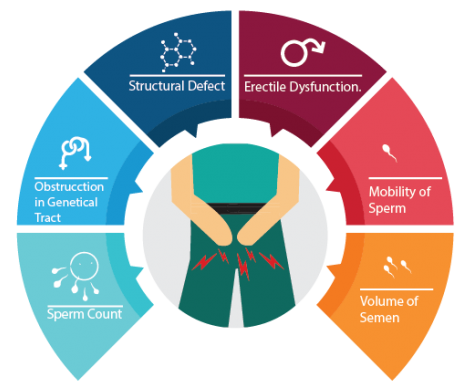
Male factor infertility refers to the failure of a couple to achieve conception due to problems specifically related to the man’s sperm, seminal fluid or reproductive organs. A number of things can affect sperm count, ability to move (motility) or ability to fertilize the egg. The most common causes of male infertility include:
- Abnormal sperm production or function
- Problems with the delivery of sperm due to sexual problems, such as erectile dysfunction, premature ejaculation, ejaculatory incompetence , retrograde ejaculation; or blockage of the part of the testicle that contains sperm (epididymis) or scarring from genital infections
- General health and lifestyle issues such as poor nutrition, obesity, stress or use of alcohol, tobacco and drugs
- Over-exposure to certain environmental hazards and toxins, such as pesticides, lead, paint, radiation, radioactive substances, mercury, benzene, boron, and heavy metals
- Ageing male – Men older than age 40 may be less fertile than younger men
Male Infertility Diagnosis
Tests for male infertility attempt to determine whether any of these processes are impaired.
General physical examination – This includes examination of your genitals and questions concerning your medical history, illnesses and disabilities, medications and sexual habits.
Semen analysis – This is a very important test for the male partner. Your doctor may ask for one or more semen specimens. Semen is generally obtained by masturbating or by interrupting intercourse and ejaculating your semen into a clean container. A laboratory analyzes your semen specimen for quantity, colour and presence of infections or blood.
Hormone testing – A blood test to determine the level of testosterone and other male hormones is common.
Doppler evaluation of the testis and Transrectal Ultrasound – Doppler/Ultrasound can help your doctor look for evidence of conditions such as retrograde ejaculation and ejaculatory duct obstruction
Male Infertility Treatments
Treatment of male infertility depends on the cause, period of infertility, age, your partner’s age and many personal preferences.
Simple lifestyle changes
Abstaining from alcohol, tobacco and illicit drugs can improve male fertility. A healthy diet, sufficient (not excessive) exercise, proper amounts of vitamin B12, vitamin C and zinc also improve fertility.
General sexual problems
Addressing impotence or premature ejaculation can improve fertility. Treatment for these problems often is primarily with medication or behavioural approaches, though mechanical and surgical treatments are sometimes effective. Artificial insemination with an ejaculate could be deployed to overcome infertility.
Low sperm counts
Hormonal treatment is needed usually in 5% of the men. Other treatments include surgical treatment of varicocele, ejaculatory duct incisions and sperm concentration methods through electroejaculation.
In absent sperms
Microsurgical bypass operations, micro-epididymal sperm aspiration (MESA) and bilateral testicular biopsies are the treatment procedures that are commonly deployed.
Therapeutic donor insemination (TDI) is a sound option for many causes of male infertility This treatment is carried out in cases of irreversible azoospermia, severe oligospermia, poor motility and abnormal morphology of sperm. Other cases include reproductive option after radiation or chemotherapy, severely Rh-sensitized and Rh-negative women with an Rh-positive partner.
Medical Management
At NewLife Advanced Fertility Center Fertility, we provide individual care to all our patients and ensure that appropriate treatment, medication and advice is available throughout the treatment lifecycle.
Surgical Management
Surgical sperm retrieval is indicated when there is no sperm in the ejaculate (azoospermia). This can result from an obstruction in the reproductive tract (obstructive azoospermia) or due to lack of sperm production (non-obstructive azoospermia). Obstructive azoospermia may be due to a blockage of the tubes transporting the sperm (due to infection or due to surgical blockage of the vas following the male sterilization). Surgical sperm retrieval techniques enable the urologist to recover sperm directly from the epididymis or even the testes of men with obstructive azoospermia so that the sperm can then be used to fertilize eggs by ICSI. The extra sperm and testicular tissue can be frozen for future attempts.
Sperm Retrieval
Reproductive Surgery (Micro Surgery) – Surgical sperm retrieval can be achieved by:
Percutaneous Epididymal Sperm Aspiration (PESA)
Microsurgical Epididymal Sperm Aspiration (MESA)
Microsurgical epididymal sperm aspiration is performed as an open operation under the operating microscope. Individual tubules of the epididymis are isolated and micropuncture aspiration is taken. This approach has the advantages of reliable retrieval of large numbers of epididymal spermatozoa that can be readily frozen and thawed for subsequent attempts at fertility. Since MESA involves direct retrieval of spermatozoa from the epididymal tubule, it minimizes the contamination of the epididymal fluid by blood cells which may affect spermatozoa fertilizing capacity during the IVF.
Testicular Sperm Aspiration (TESA)
Testicular fine-needle aspiration of the testis is done for the recovery of spermatozoa. Percutaneous puncture and aspiration of the testis can be performed using a 21-23-gauge needle connected to a 20cc syringe.
Testicular Sperm Extraction (TESE)
Under local or general anesthesia, sperm retrieval is effected using an open testicular biopsy technique.
Fertility Assessment Packages
- ED Screening
- Female fertility Assessment
- Male fertility Assessment
- Men’s Sexual Health Assessment
There are many different factors that can affect the fertility of both women and men. Even if you are not currently trying for a baby you may be wondering, or have concerns about your fertility health. There are various screening tests that can be done to evaluate fertility for both women and men.
At NewLife AdvanceFertility Center, we offer a Fertility Assessment to look at some of these key issues, hopefully at an early stage when any problems found can be investigated in detail and acted on, (we know from experience that many patients, to their cost, spend several years being slowly investigated and only seek specialist help when time is running out).
Important Note: The Fertility Assessment is designed to give an indication of lifestyle and other health issues, which may have a bearing on an individual’s, or a couple’s fertility health. The tests are not intended to replace formal comprehensive diagnostic testing, and further diagnostic testing may be advised, once the Fertility Assessment results are known.